Team headed by Dr. Brian Chicoine from the Adult Down Syndrome Center in Park Ridge, IL, reviewed records from “up to 28 years of data, compiled from 6078 individuals with DS” and a similar group without Ds, to determine what conditions are more prevalent in the Ds population.
read moreResearchers, including clinicians from the Jérôme Lejeune Institute and the University of Chicago, recently published a paper on the possibility of a link between stress and the onset of dementia in patients with Down syndrome (Ds).
read moreA recent study from Sweden looks at whether adults with Down syndrome adhere to medical guidelines. Specific medical guidelines for health surveillance exist for people with Down syndrome (DS) since 25 years but knowledge of adherence to the guidelines is lacking. The guidelines…
read moreA recent study from Turkey examined the eating habits of 20 people who have Down syndrome. Even though the study represents a different culture, it is always interesting to learn from any information that exists, especially when it comes to adults with…
read moreThis new research study looks at the causes of death for people with intellectual disabilities and specifically adults with Down syndrome. Important facts: “for Down syndrome adults ‘Down syndrome’,and dementia were most common.” [cause of death] [people with intellectual disabilities] “die younger,…
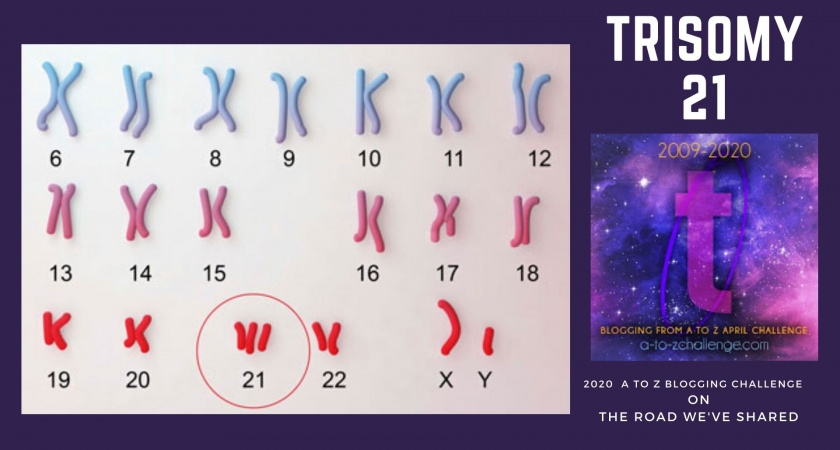
read moreTrisomy 21 – a.k.a. Down syndrome. Let’s talk DS.
read moreSelf-isolation can bring increased anxiety, depression, loneliness and other mental health issues. How do you combat the staying-inside-blues? Natalie Weston dances with her brother, Jake who has been self-isolating for a week, through a glass window. She posted a video on her…
read moreDown Syndrome in Adults Success and Challenge
read moreYou never know what you might learn in National Down Syndrome Awareness Month, IF you keep your eyes and mind open.
read moreScientists say people with Down syndrome have different needs when it comes to cancer screening.
read more